The European Society of Hypertension (ESH)/International Society of Hypertension (ISH) from April 11 to 14, 2021 is in full swing, and the meeting will interpret the latest “2021 Practical Guidelines for Outdoor Blood Pressure Measurement in ESH Clinics and Clinics”. Here is a brief overview of the guide content.
| Clinical Application | Clinic | Home | 24h Ambulatory | Pharmacy | Public Place |
| Screening | +++ | + | – | ++ | + |
| Initial Diagnosis | + | ++ | +++ | – | – |
| Titration of Medication | + | ++ | ++ | – | – |
| Follow-up | ++ | +++ | + | + | – |
| Main Indications | Screening of untreated patients; Follow-up of treated patients | Long-term follow-up of treated patients (preferred method) | Initial diagnosis (preferred method) | Screening of untreated patients; Follow-up of treated patients | Opportunistic screening |
| Blood Pressure (mmHg) | ≥ 140/90 | ≥ 135/85 | ≥ 130/80 | ≥ 135/85 (awaiting research) | / |
Explanation of the symbols:
- +++: Highly recommended/Applicable
- ++: Recommended/Applicable
- +: May be considered/Applicable
- -: Not recommended/Not Applicable
- / : Not specified or not applicable
1, Blood pressure measurement
1) Blood pressure measurement equipment
Use standard and verified blood pressure measurement equipment.
In 2018, the American Association of Medical Instrumentation (AAMI), the European Society of Hypertension (ESH), and the International Standard Organization (ISO) jointly developed a unified AAMI/ESH/ISO blood pressure meter accuracy verification program.
Verified electronic blood pressure devices in adults may be inaccurate in special populations (children, pregnant women, arm circumference > 42 cm, arrhythmias, especially patients with atrial fibrillation).
2) Cuffs for blood pressure measurement devices
Choosing a cuff that fits the arm circumference is crucial for accurate blood pressure measurement. A smaller size will overestimate blood pressure, while a larger size will underestimate blood pressure.
Manual stethoscope device: The cuff length is 75% to 100% of the circumference of the middle of the upper arm, and the cuff width is 37% to 50% of the circumference of the upper arm.
Automated electronic equipment: Select the appropriate cuff size according to the operating instructions of the device.
Conical cuffs are more suitable for patients with arm circumference > 42 cm, because rectangular cuffs may overestimate blood pressure.
The center of the air bag should be placed at the brachial artery pulse in the antecubital fossa.
The lower end of the cuff should be 2-3 cm above the antecubital fossa. The top and bottom edges of the cuff should be loose and suitable for accommodating a finger underneath.
2, White coat hypertension and masked hypertension
According to the results of office and out-of-office blood pressure (HBPM or ABPM) measurements, patients can be divided into four categories:
1) Normal blood pressure: neither office nor out-of-office blood pressure is elevated; 2) Persistent hypertension: both office and out-of-office blood pressure are elevated; 3) White coat hypertension (WCH): office blood pressure is elevated, but out-of-office blood pressure is not high; 4) Masked hypertension (MH): out-of-office blood pressure is elevated, but office blood pressure is not high.
| White-Coat Hypertension | Masked Hypertension | |
| Diagnosis | Clinic blood pressure is elevated, but out-of-office blood pressure is not high. | Out-of-office blood pressure is elevated, but clinic blood pressure is not high. |
| Management | Improve lifestyle, annual follow-up. Patients with high or very high cardiovascular risk should consider drug treatment. | Improve lifestyle and consider drug treatment. |
The diagnosis of white coat hypertension and masked hypertension requires a second out-of-office blood pressure measurement to confirm.
When the office blood pressure approaches 140/90 mmHg, misdiagnosis increases.
When the office blood pressure is 140-159/90-99 mmHg, home blood pressure monitoring or dynamic blood pressure monitoring is strongly recommended;
When the office blood pressure is 130-139/85-89 mmHg, the possibility of masked hypertension is high, and out-of-office blood pressure assessment is strongly recommended.
In some special cases (such as pregnant women, children and patients with chronic kidney disease), out-of-office blood pressure monitoring is particularly important for diagnosis and follow-up.
3, Office blood pressure measurement
1) Office blood pressure measurement steps
- No Smoking, Drinking Coffee, Eating, and Exercising for 30 Minutes Before Measurement.
- Room Quiet.
- Suitable Temperature.
- Rest for 3-5 Minutes.
- Avoid Talking During Blood Pressure Measurement.
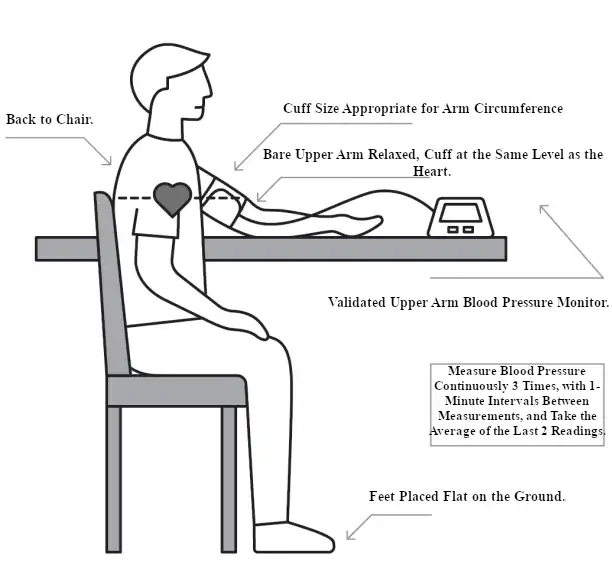
2) Diagnosis of hypertension based on office blood pressure
It is usually necessary to measure at least 2-3 times within 1-4 weeks to evaluate office hypertension.
Hypertension should not be diagnosed based on a single office blood pressure unless the office blood pressure is ≥ 180/110 mmHg and there is evidence of target organ damage or cardiovascular disease.
In most cases, hypertension should be diagnosed by home blood pressure monitoring or dynamic blood pressure monitoring. If home blood pressure monitoring or dynamic blood pressure monitoring is not possible, multiple office blood pressure measurements are required to diagnose hypertension.
3) Difference in blood pressure between the upper arms
At the first visit, blood pressure in both arms should be measured.
If the difference in blood pressure between the arms is > 10 mmHg, repeated measurements should be performed to confirm; in this case, the higher blood pressure value should be used.
If the difference in blood pressure between the arms is > 20 mmHg, arterial disease screening should be performed.
4) Standing blood pressure
In patients with hypertension, standing blood pressure should be measured in addition to sitting blood pressure.
Standing blood pressure should be measured if symptoms suggest postural hypotension, especially in the elderly and patients with degenerative diseases (such as Parkinson’s disease, dementia) or diabetes.
Measure blood pressure after standing for 1 minute and again after 3 minutes.
If systolic blood pressure drops by ≥ 20 mmHg within 3 minutes, postural hypotension is present.
5) 24-hour dynamic blood pressure monitoring
24-hour dynamic blood pressure monitoring is used to evaluate the 24-hour blood pressure control of antihypertensive drug therapy. It helps to identify white coat hypertension and masked hypertension. Its indications are as follows:
① Preliminary diagnosis
• Used to diagnose hypertension;
• Used to screen white coat hypertension and masked hypertension;
• Used to identify nocturnal hypertension and non-dipper hypertension;
• Used to evaluate blood pressure changes caused by autonomic failure.
② Treated hypertension
• Used to identify white coat hypertension and masked hypertension;
• Confirm the diagnosis of uncontrolled and refractory hypertension;
• Ensure 24-hour blood pressure control (especially high-risk patients and pregnant women);
• Used to confirm hypotension caused by overtreatment;
• Used to evaluate nocturnal hypertension and non-dipper hypertension;
• Inconsistency between office blood pressure and out-of-office blood pressure diagnosis.
③ When to repeat monitoring
• Used to ensure adequate blood pressure control, especially in patients with increased risk of cardiovascular disease;• Uncontrolled hypertension: May be monitored once every 2 to 3 months until 24-hour blood pressure is normal;
• Controlled hypertension: May be monitored once a year.
4, Home blood pressure measurement
Home blood pressure monitoring helps identify white coat hypertension and masked hypertension, and is the best method for long-term follow-up of hypertension treatment.
1) Clinical indications for home blood pressure monitoring
① Preliminary diagnosis
• Used to confirm hypertension;• Used to screen for white coat hypertension and masked hypertension.
② Treated hypertension
• Used in all hypertensive patients receiving treatment;• Identify white coat hypertension and masked hypertension;
• Used to titrate antihypertensive drugs;
• Used to monitor long-term blood pressure control;
• Ensure strict blood pressure control (high-risk patients, pregnant women, etc.);
• Used to improve patients’ long-term treatment compliance.
2) Home blood pressure monitoring plan
① Used for diagnosis and before each visit
• Measure for 7 days (at least 3 days);
• Measure in the morning and evening;
• Measure before meals, and before taking medication if receiving antihypertensive treatment;
• Measure 2 times each time, with an interval of 1 minute.
② Long-term follow-up of hypertension treatment
• Repeat measurement 1-2 times a week (most frequent) or monthly (minimum requirement)
The effectiveness and applicability of blood pressure measurement in pharmacies have not been fully studied. 24-hour dynamic blood pressure monitoring can be performed in pharmacies.
There are few studies on blood pressure measurement in public places, but it is helpful for screening of the general population.
The accuracy and practicality of cuffless wearable blood pressure monitoring are still uncertain, so it should not be used for the diagnosis and treatment of hypertension.
